With Behavioral health coverage in health plans at the forefront, this paragraph opens a window to an amazing start and intrigue, inviting readers to embark on a storytelling journey filled with unexpected twists and insights.
Behavioral health coverage in health plans is crucial for ensuring individuals have access to necessary mental health services. From understanding what services are covered to exploring the impact of comprehensive coverage, this topic delves into the complexities of behavioral health care within health plans.
Overview of Behavioral Health Coverage

Behavioral health coverage in health plans refers to the inclusion of services that address mental health and substance abuse disorders. This coverage is essential for ensuring individuals have access to the necessary care and treatment to address their behavioral health needs.
Examples of Common Mental Health Services Covered
- Counseling and therapy sessions with licensed mental health professionals.
- Patient education and support groups for individuals dealing with mental health issues.
- Psychiatric evaluations and medication management for mental health conditions.
- Inpatient and outpatient treatment programs for substance abuse disorders.
Importance of Including Behavioral Health Coverage
Behavioral health coverage is crucial as it helps individuals receive the care they need to manage and improve their mental health. By including behavioral health benefits in health plans, individuals are more likely to seek treatment and support, leading to better overall health outcomes. Additionally, addressing mental health issues early can prevent more severe conditions from developing, ultimately reducing healthcare costs in the long run.
Types of Behavioral Health Services Covered: Behavioral Health Coverage In Health Plans

When it comes to behavioral health services covered by health plans, there is a range of options available to individuals seeking treatment for mental health issues. These services can vary from therapy sessions to more intensive treatments depending on the individual’s needs.
Different Types of Behavioral Health Services
- Individual Therapy: One-on-one sessions with a therapist to discuss and work through personal issues.
- Group Therapy: Sessions with a group of individuals led by a therapist to address shared concerns and provide support.
- Family Therapy: Therapy sessions involving family members to improve communication and resolve conflicts.
- Medication Management: Oversight and management of psychiatric medications by a healthcare provider.
- Intensive Outpatient Programs (IOP): Structured programs that offer more frequent therapy sessions without requiring overnight stays.
- Inpatient Treatment: Residential treatment for individuals requiring 24-hour care in a hospital or specialized facility.
Difference between Inpatient and Outpatient Behavioral Health Services
Outpatient behavioral health services are typically less intensive and allow individuals to continue their daily activities while receiving treatment. In contrast, inpatient services involve round-the-clock care in a controlled environment, often for more severe cases or crises.
When it comes to choosing a health insurance plan, understanding the details of PPO health insurance coverage explained is crucial. With a PPO plan, you have the flexibility to see any doctor or specialist without a referral, but staying in-network can save you money on out-of-pocket costs. To learn more about how PPO plans work, check out this informative guide on PPO health insurance coverage explained.
Specific Therapies or Treatments Covered
- Cognitive Behavioral Therapy (CBT): A form of therapy that helps individuals identify and change negative thought patterns and behaviors.
- Dialectical Behavior Therapy (DBT): A type of therapy that focuses on regulating emotions and improving interpersonal relationships.
- Exposure Therapy: A treatment method that involves gradually exposing individuals to feared objects or situations to reduce anxiety or phobias.
- Eye Movement Desensitization and Reprocessing (EMDR): A therapy technique used to process traumatic memories and alleviate associated distress.
Challenges in Behavioral Health Coverage
Accessing behavioral health services through health plans can present individuals with several challenges. These challenges can often hinder individuals from receiving the necessary care and support for their mental health needs. Disparities in coverage between mental health and physical health treatments, as well as limited behavioral health coverage in some health plans, further compound these challenges.
Disparities in Coverage
- Many health plans offer limited coverage for mental health treatments compared to physical health treatments.
- Some plans may have higher copayments, deductibles, or restrictions for mental health services, making them less accessible.
- Insurance companies may also have stricter criteria for approving mental health treatments, leading to delays or denials of coverage.
Reasons for Limited Coverage
- Historical stigma surrounding mental health may have influenced the development of health plans with limited coverage for behavioral health services.
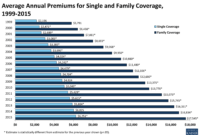
- Cost considerations play a significant role, as mental health treatments can be expensive, leading some health plans to restrict coverage to control costs.
- Insufficient provider networks specializing in behavioral health can also limit coverage options for individuals seeking mental health services through their health plans.
Impact of Comprehensive Behavioral Health Coverage

Comprehensive behavioral health coverage can have a transformative impact on individuals, communities, and society as a whole. By ensuring access to a wide range of mental health and substance abuse services, such coverage plays a crucial role in improving overall well-being and quality of life.
Potential Benefits for Individuals
- Early intervention and treatment for mental health issues, leading to improved outcomes and recovery.
- Reduced stigma surrounding seeking help for behavioral health concerns.
- Enhanced coping skills and resilience, resulting in better emotional regulation and stress management.
Improved Well-being and Quality of Life, Behavioral health coverage in health plans
- Increased productivity and engagement in work, school, and relationships.
- Decreased risk of developing chronic physical health conditions associated with untreated mental health disorders.
- Enhanced ability to navigate life challenges and maintain overall wellness.
Positive Impact on Communities
- Reduced burden on emergency services and healthcare systems due to preventative care and early intervention.
- Stronger social connections and support networks, fostering a sense of belonging and community resilience.
- Higher rates of treatment completion and recovery, leading to lower rates of substance abuse and related crimes.
In conclusion, Behavioral health coverage in health plans plays a vital role in promoting overall well-being and improving quality of life. By addressing challenges and disparities, comprehensive coverage can positively impact individuals and communities alike, highlighting the importance of prioritizing mental health within health plans.
High deductible health plans (HDHP) are becoming increasingly popular due to their lower monthly premiums. However, it’s important to understand how these plans work and what expenses you may be responsible for before choosing one. To delve deeper into the details of HDHPs and whether they’re the right choice for you, read this comprehensive article on High deductible health plans (HDHP).
For individuals with pre-existing conditions, finding adequate health insurance coverage can be challenging. Understanding your options and rights when it comes to coverage for pre-existing conditions is essential for ensuring you receive the care you need. To learn more about how to navigate this complex issue, visit this resource on Coverage for pre-existing conditions.